Cardioversion is a medical procedure that restores a normal heart rhythm in people with certain types of abnormal heartbeats (arrhythmias). Cardioversion is usually done by sending electric shocks to your heart through electrodes placed on your chest. It’s also possible to do cardioversion with medications.
Cardioversion is usually a scheduled procedure that’s performed in a hospital under sedation. You should be able to go home the same day as your procedure. For most people, cardioversion quickly restores a normal heart rhythm.
Cardioversion is different from defibrillation, an emergency procedure that’s performed when your heart stops or quivers uselessly. Defibrillation delivers more powerful shocks to the heart to correct its rhythm.
Preparation: Cardioversion procedures are usually scheduled in advance, although if your symptoms are severe, you may need to have cardioversion in an emergency setting. You can’t eat or drink anything for about 8 hours before your procedure. Your doctor will tell you whether you should take any of your regular medications before your procedure. Before cardioversion, you may have a procedure called a transesophageal echocardiogram (TEE) to check for blood clots in your heart, which can be dislodged by cardioversion, causing life-threatening complications.
In a transesophageal echocardiogram, your throat is numbed and a flexible tube containing a transducer is guided down your throat and into your oesophagus. From there, the transducer can obtain more-detailed images of your heart so that your doctor can check for blood clots.
Procedure
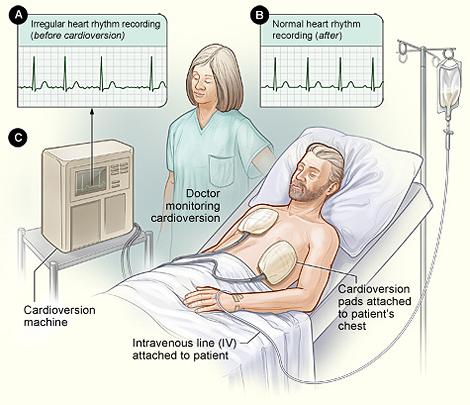
A nurse or technician will place several large patches called electrodes on your chest. The electrodes will be connected to a cardioversion machine (defibrillator) using wires.
The defibrillator will record your heart rhythm throughout the procedure and will deliver shocks to your heart to restore a normal heart rhythm. This machine can also correct your heart’s rhythm if it beats too slowly after cardioversion.
Before the shocks are delivered, a nurse or technician will insert an intravenous (IV) line in your arm. The IV line is used to give you medications that will make you sleep
during the procedure so that you won’t feel any pain from the shocks. Your doctor may also use the IV line to give you additional medications that can help restore your heart rhythm.
Once you’re sedated, electric cardioversion usually only takes a few minutes to complete.
After the procedure
Electric cardioversion is done on an outpatient basis, meaning you can go home the same day your procedure is done. You’ll spend an hour or so in a recovery room being closely monitored for complications. Because you’ll be asleep for the procedure, your awareness of your surroundings may be affected afterward. You’ll need someone to drive you home, and your ability to make decisions may be affected for several hours after your procedure.
Even if no clots were found in your heart before your procedure, you’ll take blood-thinning medications for at least several weeks after your procedure to prevent new clots from forming.
Risks
Complications of electric cardioversion are uncommon, major risks of cardioversion include:
- Dislodged blood clots. Some people who have irregular heartbeats have blood clots in their hearts. Electric cardioversion can cause these blood clots to move to other parts of your body. This can cause life-threatening complications, such as a stroke or a blood clot traveling to your lungs (pulmonary embolism).
- Abnormal heart rhythm. In rare cases, some people who undergo cardioversion end up with other heart rhythm problems during or after their procedure. This is a rare complication. If it happens, it usually shows up only minutes after your procedure, so your doctor can give you medications or additional shocks to correct the problem.
- Skin burns. Rarely, some people have minor burns on their skin where their electrodes were placed.
Pregnant women can have cardioversion, but it’s recommended that the baby’s heartbeat is monitored during the procedure.